PICC (Peripherally Inserted Central Catheter) Insertion Technique
Posted by Dr KAMAL DEEP on December 5, 2011
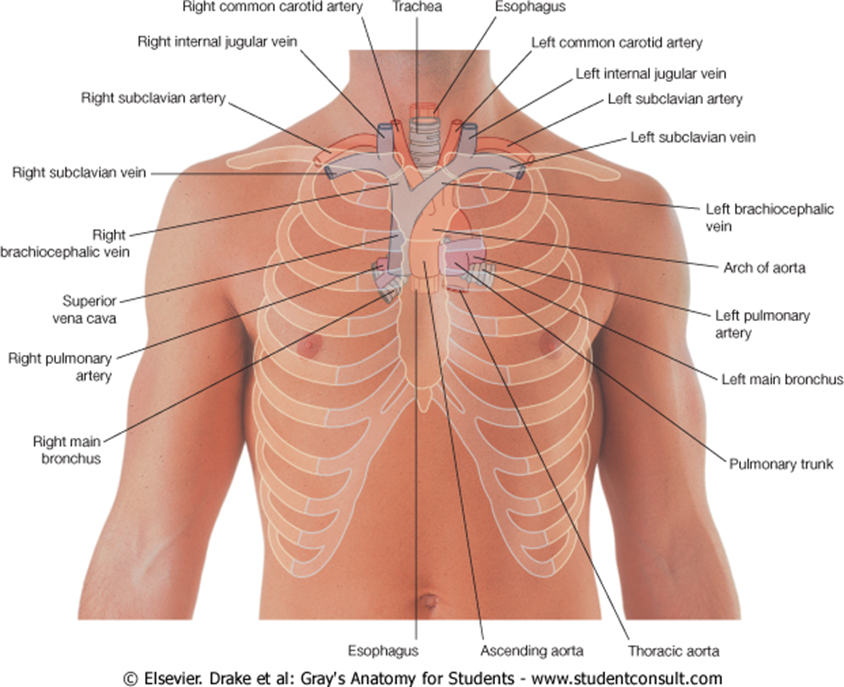
1. The insertion site (below or above the antecubital fossa), 2. The sternocleidomastoid triangle at the medial third of the clavicle, and 3. The 3rd right costosternal junction of the sternum.
sum of the two linear distances measured between the three landmarks (with the inserted arm abducting laterally at 45-degree angle from the body) is the optimal PICC length.
PICC INSERTION TECHNIQUE
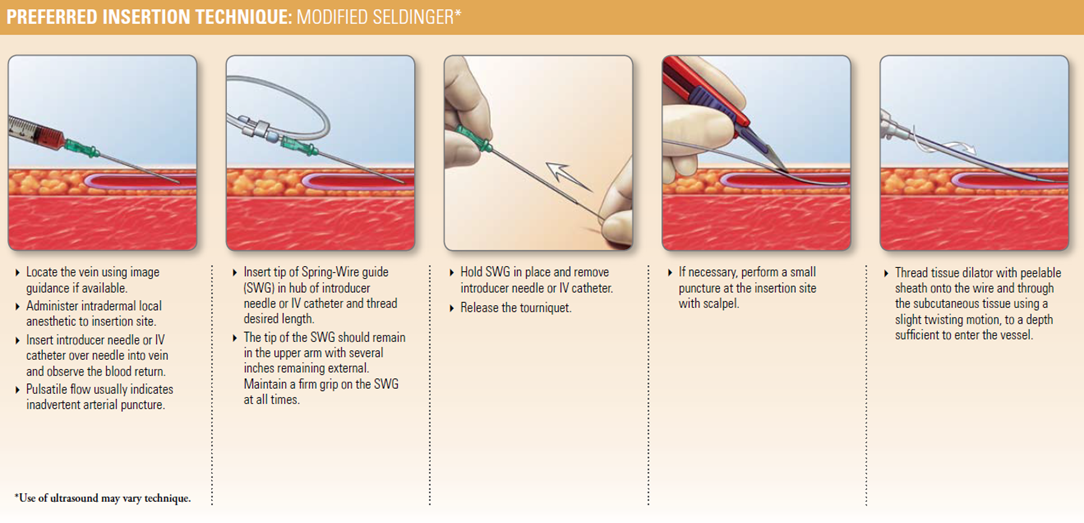
1. Guidewire / SWG Insertion Techniques:
Kits/Sets are available with a variety of Guidewires/SWGs. Guidewires are provided in different diameters, lengths, and tip configurations for specific insertion techniques. Become familiar with the guidewire(s) to be used with the specific technique chosen, before beginning the actual PICC insertion procedure.
Image guidance may be used to gain initial venous access.
Catheter Insertion with an 80 cm Guide wire:
Use single 45 cm guidewire for venous access and 80 cm soft tip guidewire for catheter placement. Image guidance or fluoroscopy is used to gain initial venous access; catheter placement with 80 cm guidewire is done under fluoroscopy.
• Gain venous access with 45 cm guidewire and peel-away sheath.
• Load PICC onto 80 cm guidewire until soft tip of wire extends beyond tip of catheter.
• While maintaining control of distal end of guidewire, advance soft tip/catheter tip as a unit through peel-away sheath to desired depth.
• Once catheter is in desired location, remove guidewire.
Catheter Insertion with an 130 cm Guidewire:
Use single 45 cm guide wire for venous access and 130 cm soft tip guidewire for catheter placement. Image guidance or fluoroscopy is used to gain initial venous access; catheter placement with 130 cm guidewire is done under fluoroscopy.
• Gain venous access with 45 cm guidewire.
• Insert soft end of 130 cm guidewire through peel-away sheath to desired depth.
• Thread catheter over guidewire and advance catheter over guidewire through sheath into vessel into correct position.
• Once catheter is in desired location, remove guidewire.
NOTE: Some clinicians will gain access with 130 cm guide wire and thread catheter over guide wire once wire has been correctly positioned in the SVC. This technique is done under fluoroscopy.
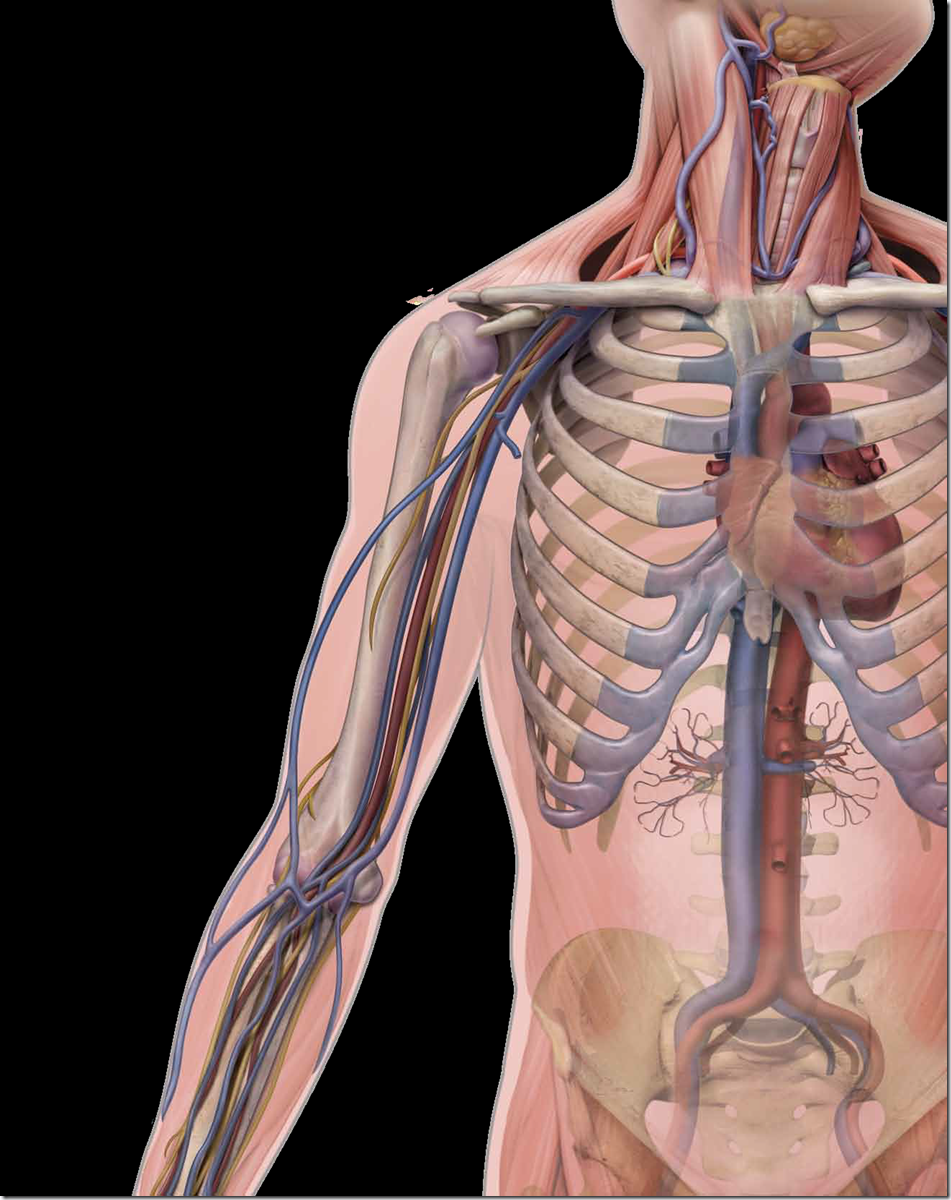
Identify insertion vein:
• Apply tourniquet above anticipated insertion vein.
• Identify appropriate vein for insertion. Use direct visualization technologies, if available, and assess vein health.
5. Release tourniquet and leave in place beneath the arm.
6. Measure patient to assure placement of catheter in the SVC:
• Extend arm laterally 45 to 90 degrees from trunk.
• Measure distance from insertion site along presumed anatomical course of vessel to be catheterized.
• Catheter tip should lie in distal one-third of SVC above right atrium and parallel to SVC wall.
◊ If a catheter stabilization device will be used, add ½ to 1 inch (1.2 to 2.5 cm) to catheter measurement (STATLOCK®); if another device is used, check manufacturer recommendations.
◊ If using upper arm circumference assessment; for consistency in measurement, measure from an anatomical point and record.
7. Position patient as appropriate for insertion site:
• Extend arm laterally 45 to 90 degrees from trunk.
8. Prepare work area.
2. Prep Puncture Site:
1. Prep and drape peripheral puncture site.
2. Perform skin wheal with a local anesthetic as needed.
3. Gain Initial Venous Access:
See specific guidewire instructions, Guidewire Insertion Techniques (page 7) under Accessory Component Instructions section.
1. Insert soft tip of guidewire through introducer needle into vein. Advance guidewire to desired depth.
Warning: Do not insert stiff end of soft tip guidewire into vessel as this may result in vessel damage.
Warning: Do not cut guidewire to alter length.
Warning: Do not withdraw guidewire against needle bevel to minimize the risk of possible severing or damaging of guidewire.
2. Remove needle:
Hold guidewire in place while removing introducer needle.
Caution: Maintain firm grip on guidewire at all times.
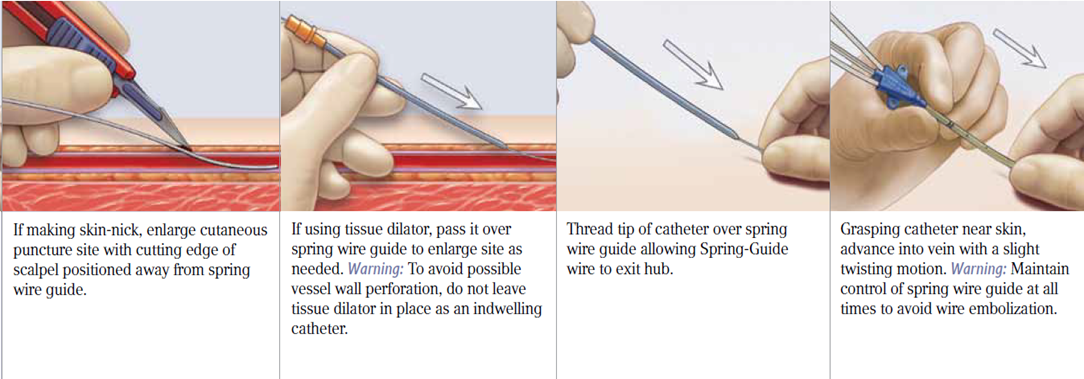
3. Enlarge puncture site, if necessary:
Use scalpel positioned away from the guidewire to enlarge cutaneous puncture site. Do not cut guidewire. Retract scalpel to the protected position.
4. Sheath Placement:
1. Thread tapered tip of peel-away sheath/dilator assembly over guidewire. Grasping near skin advance assembly with slight twisting motion to a depth sufficient to enter vessel. Dilator may be partially withdrawn to further facilitate advancement of sheath into the vessel. A slight twisting motion of the peel-away might help sheath advancement.
Caution: Do not withdraw tissue dilator until the sheath is well within the vessel to minimize the risk of damage to sheath tip. Sufficient guidewire length must remain exposed at hub end of sheath to maintain a firm grip on guidewire.
2. Check sheath placement by holding sheath in place, withdraw guidewire and dilator sufficiently to allow venous blood flow. Holding sheath in place, remove guidewire and dilator as a unit.
Warning: Do not leave the dilator in place as an indwelling catheter to minimize the risk of possible vessel wall perforation.
Warning: Do not apply undue force on guidewire to minimize the risk of possible breakage.
5. Catheter Advancement:
Advance catheter according to the guidewire used. Review detailed instructions for 80 cm and 130 cm guidewire usage (page 7) under Accessory Component Instructions section.
Warning: Do not apply excessive force in placing or removing catheter. Failure to do so can result in catheter breakage. If placement or withdrawal cannot be easily accomplished, an x-ray should be obtained and further consultation requested.
1. Retract catheter guard.
2. Insert catheter through peel-away sheath.
• If resistance is met while advancing catheter, retract and/or gently flush while advancing.
3. Stop advancing catheter 5 inches (13 cm) before reaching pre-established insertion length.
4. Withdraw peel-away sheath over catheter until free from venipuncture site.
5. Grasp tabs of peel-away sheath and pull apart, away from catheter, until sheath splits down entire length.
6. Advance catheter to final indwelling position.
Placement Wire (where provided):
Caution: To minimize the risk of placement wire kinking, do not clamp extension line(s) when placement wire is in catheter.
1. Complete catheter insertion.
2. Remove placement wire.
Warning: Remove placement wire and Luer-Lock sidearm assembly as a unit (see Figure 24). Failure to do so may result in wire breakage.
6. Dressing:
Replace dressing according to organizational policies, procedures, and practice guidelines. Change immediately if the integrity becomes compromised e.g. dressing becomes damp, soiled, loosened, or no longer occlusive.
• Consult manufacturer’s recommendations for dressing specifics.
• Transparent semipermeable membrane dressing should be changed every 7 days.
• Gauze and tape should be changed every 48 hours.
• Label dressing with type, size, and length of catheter; date and time; and initials of the clinician performing dressing change.
7. Maintain Catheter Patency:
Maintaining central venous catheter patency shall be done in accordance with organizational policies, procedures, and practice guidelines. All personnel who care for patients with central venous catheters must be knowledgeable about effective management to prolong catheter’s dwell time and prevent injury.
Perform hand hygiene as required.
1. Solution and frequency of flushing a venous access catheter should be established in hospital/agency policy.
2. Catheter patency is established and maintained by:
• flushing intermittently via syringe with heparinized saline or preservative-free 0.9% sodium chloride (USP)
• continuous drip
• positive pressure device
3. The amount of heparin:
• depends on physician preference,
• hospital/agency protocol,
• patient condition
Caution: Assess patient for heparin sensitivity. Heparin-induced thrombocytopenia (HIT) has been reported with the use of heparin flush solutions.
The volume of flush solution should be:
• equal to at least twice the priming volume of the catheter and any add-on devices
Catheter priming volume is printed on product packaging.
5. When using any central venous catheter for intermittent infusion therapy, proper flushing (heparinization) using a positive-pressure flushing technique will help prevent occlusion. Neutral as well as positive displacement valve systems have also been shown to help prevent occlusion.
6. All valves need to be properly cleansed with an appropriate antiseptic before being accessed.
7. The SASH or SAS method of flushing will help eliminate occlusions due to incompatible solutions:
• Saline • Administer drug • Saline • Heparin (if used)
8.Catheter Removal Procedure
1. PICC removal shall be performed:
• following order of authorized prescriber
• in accordance with organizational policies, procedures, and practice guidelines
2. A PICC shall be removed immediately upon patient assessment for:
• suspected contamination
• unresolved complication
• discontinuation of therapy
3. As indicated, place patient in supine position to minimize the risk of potential air embolism.
4. Remove dressing.
Warning: Do not use scissors to remove dressing, to minimize the risk of cutting catheter.
5. Open catheter stabilization device retainer wings and remove catheter from catheter stabilization device posts.
6. Remove catheter by slowly pulling it parallel to skin. If resistance is met when removing the catheter, catheter should not be forcibly removed and the physician should be notified.
Caution: Do not exert excessive force while removing the catheter; to minimize the risk of catheter breakage.
7. Upon removal of catheter:
• measure and inspect
• ensure entire catheter length has been removed
8. Direct pressure should be applied at site until hemostasis is achieved.
9. Apply alcohol swab to catheter stabilization device adhesive and gently lift pad off of skin (if applicable).
10. Dress insertion site. Sterile occlusive dressing should be applied and site assessed every 24 hours until site is epithelialized. Residual catheter track may remain an air entry point until completely sealed (usually 24 to 72 hrs); dependent upon amount of time catheter was indwelling.
11. Document catheter removal procedure on patient’s chart per hospital/agency protocol.
Include:
• catheter condition
• length of catheter removed
• patient’s tolerance of the procedure
• any nursing interventions needed for removal
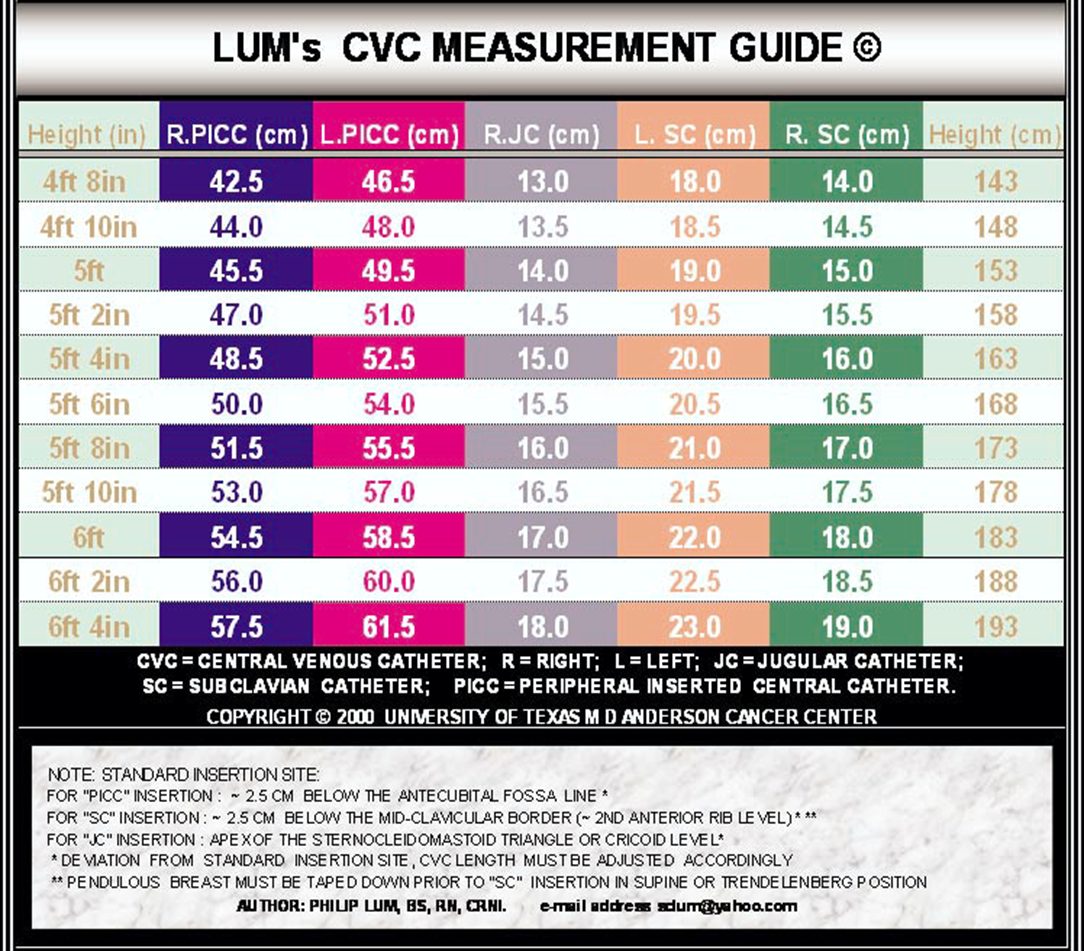
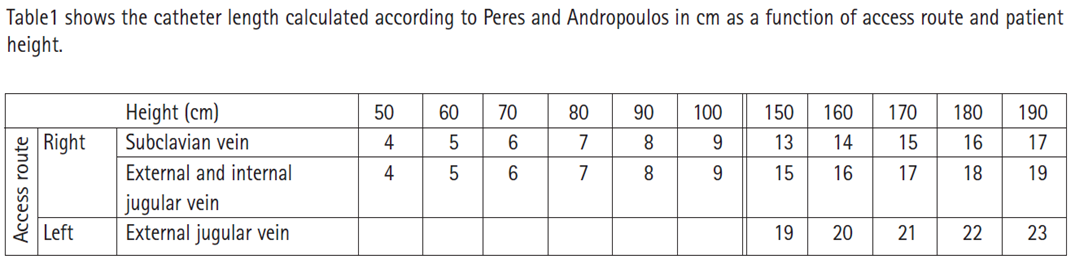
NOTE: These “standard” insertion sites were defined to correspond to the catheter lengths determined by the formulas. Any deviation from the defined site requires appropriate adjustment of catheter length. For example, a PICC inserted 2.5 cm above the antecubital fossa would be 5 cm shorter than the value from the chart, based on the patient’s height
These recommended lengths should always be critically appraised prior to use in the individual patients. For patients with unusual proportions, e.g. short or long neck, lengthy arm or upper body proportions, case-by-case decision-making is important.
Catheter Trimmer:
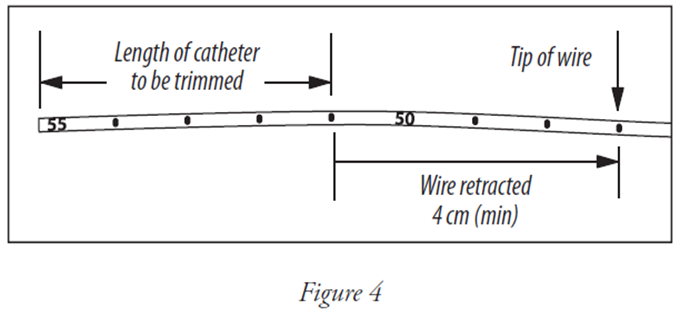
NOTE: There should be very limited resistance when cutting catheter with supplied trimmer. Any greater resistance is likely to be caused by the placement wire – which has not been sufficiently retracted. If so, do not use catheter.
Catheter Trimmer is a one time use trimming device.
• To trim catheter with Catheter Trimmer, retract placement wire 1-1/2 inches minimum (4 cm) behind where catheter is to be cut. The placement wire is to be withdrawn through septum (see Figure 4).
Kink proximal end of placement wire at connector with side-port (see Figure 5). This minimizes the risk of placement wire extending beyond distal tip of catheter during insertion. (Do not attempt to advance placement wire through septum.)
Peel back contamination guard exposing catheter portion to be trimmed. Using trimming device, cut catheter straight across (90° to catheter cross-section) to maintain a blunt tip. Warning: Do not cut placement wire when trimming catheter to minimize the risk of foreign embolism. Caution: Check that there is no wire in cut catheter segment, after trimming catheter. If there is any evidence that placement wire has been cut or damaged, catheter should not be used.
Trim Catheter:
If necessary, review detailed instructions for Catheter Trimmer device under Accessory Component Instructions section.
1. Identify catheter type:
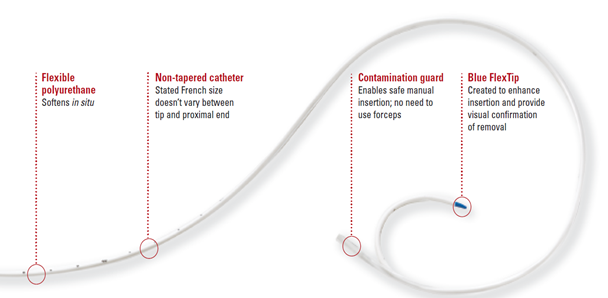
• BFT (Blue FlexTip®)
• Non-BFT
2. Peel back contamination guard exposing catheter portion to be trimmed.
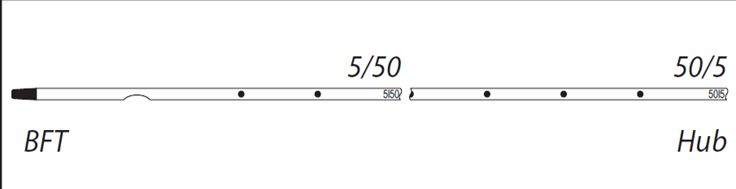
3. Review catheter marking pattern below. The catheter is marked so clinician can easily identify desired amount of catheter to be trimmed; length of catheter that remains or as with BFT catheter – both.
4. Using the trimming device, cut catheter straight across (90° to catheter cross-section) to maintain a blunt tip. NOTE: There should be very limited resistance when cutting catheter with supplied trimming device. If using a catheter with a placement wire, any greater resistance is likely to be caused by the placement wire which has not been sufficiently retracted. If so, do not use catheter. 5. Inspect cut surface for clean cut and no loose material. Warning: Do not cut placement wire when trimming catheter to minimize the risk of foreign embolism. Caution: Check that there is no wire in cut catheter segment, after trimming catheter. If there is any evidence that placement wire has been cut or damaged, catheter should not be used
BFT double numbering pattern:
◊ First number designates centimeters from tip of catheter.
◊ Second number designates centimeters from hub of catheter.
◊ This double numbering pattern permits clinician to easily identify centimeters of catheter to be trimmed and also identifies centimeters of catheter remaining.
◊ Record both numbers.
Non-BFT numbering pattern:
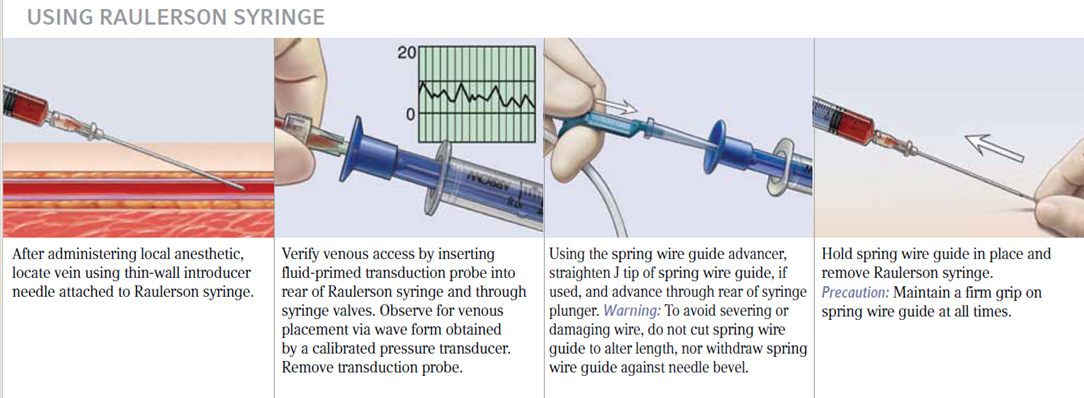
Raulerson syringe
Number designates centimeters of catheter to be trimmed and also gives amount of catheter remaining
Reducing Risks: There are two key benefits to using the Raulerson syringe. First, it lessens the exposure to blood and can lower the risk of air embolism. Second, it enables you to place the catheter in fewer steps, with less risk of dislodging needle from vessel.
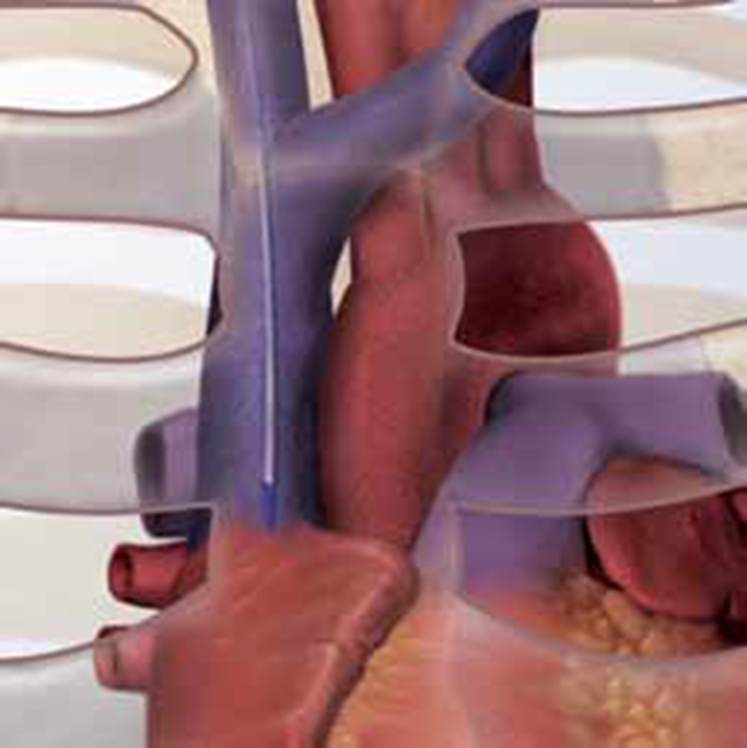
verify Catheter tip position
Based on hospital policy, utilize
one of the following methods for tip
placement verification:
• Radiographic imaging (Chest Film,
Fluoroscopy)
• Physiological Feedback such as EKG
• Other approved methods.
Appropriate tip placement for Central
Venous Catheters other than Dialysis
Catheters is in the lower one-third
of the Superior Vena Cava or at the
Cavoatrial Junction.
If catheter tip is malpositioned,
reposition and reverify tip position.
The following designations are examples for port usage and do not represent the
only way the lumens can be used:
Proximal: Blood Sampling
Medications
Blood Administration
Medial: Total Parenteral Nutrition
Medications (only if TPN use is not
anticipated)
Distal: CVP Monitoring
Blood Administration
High Volume or Viscous Fluids
Colloids
Medication
4th Lumen: Infusion
Medication
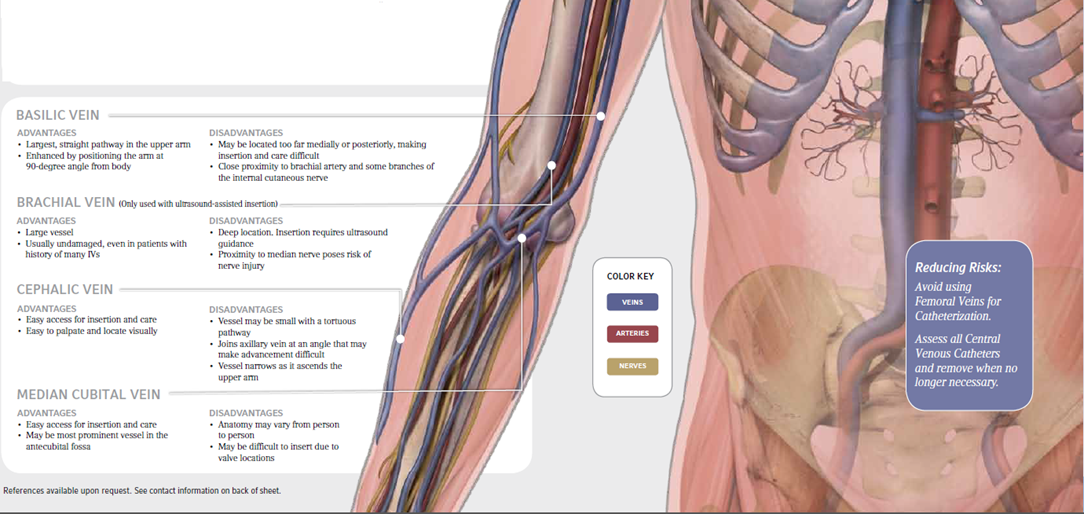
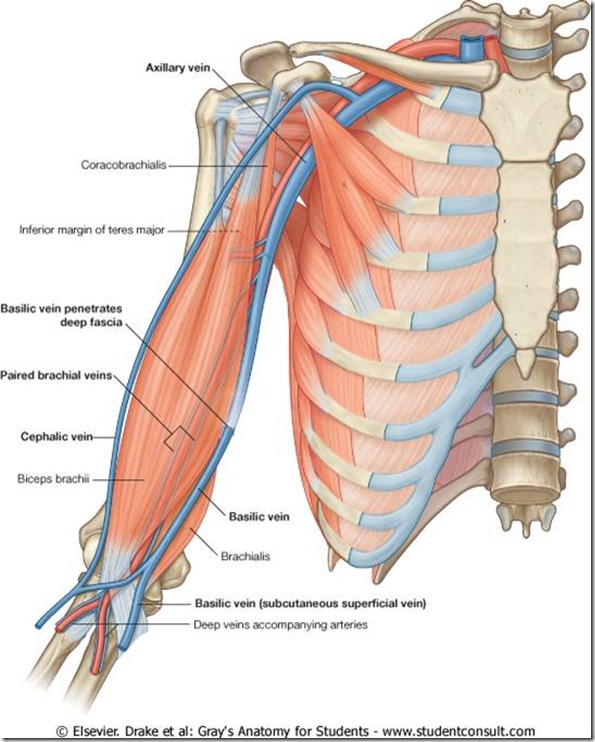
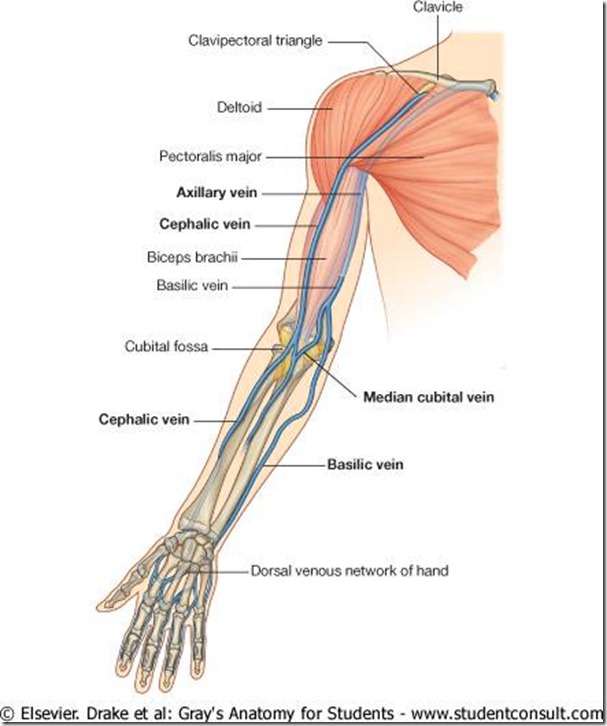
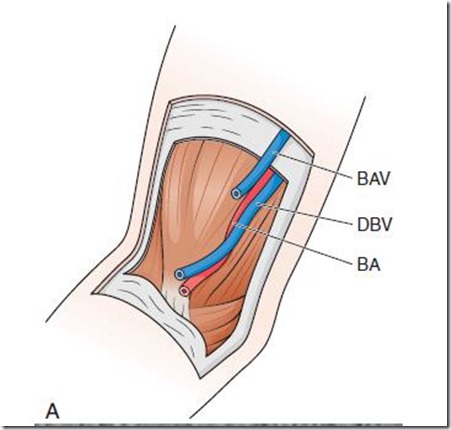
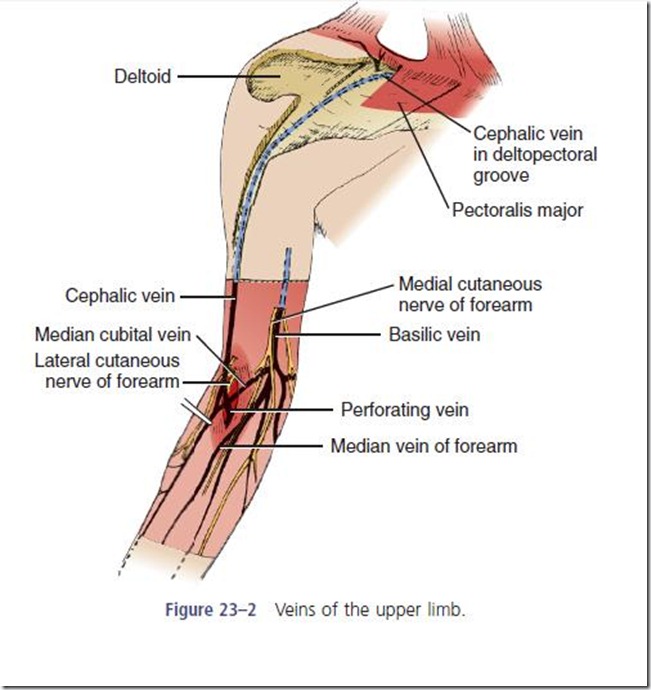
ANATOMY OF ARM VEINS
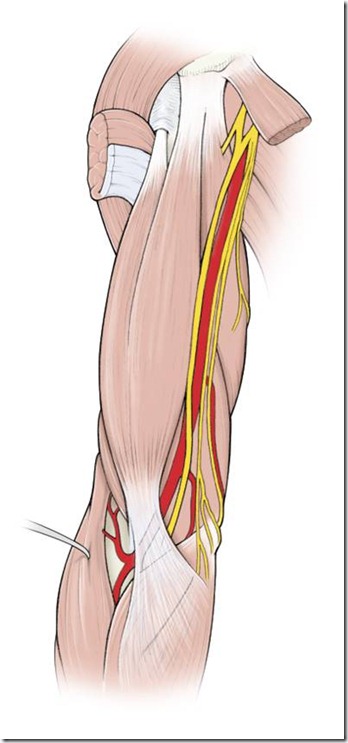
A, Anatomy of vessels in the anticubital fossa, noting
the brachial artery (BA), basilic vein (BAV), and deep brachial vein
(DBV). B, Corresponding ultrasound image. The vein collapses with
probe pressure to distinguish it from the artery.













go to my site said
you are actually a excellent webmaster. The web site loading speed is amazing.
It seems that you are doing any unique trick. Also, The contents are masterwork.
you have done a magnificent activity in this matter!
click for source said
These are actually great ideas in about blogging. You have touched
some pleasant things here. Any way keep up wrinting.
read full article said
Greetings from Ohio! I’m bored at work so I decided to browse your blog on my iphone during lunch break. I love the knowledge you provide here and can’t wait to take a look when I get home.
I’m surprised at how quick your blog loaded on my cell phone .. I’m
not even using WIFI, just 3G .. Anyhow, awesome site!
whole life companies said
Waiver Of Premium RiderWhen purchasing your whole life insurance policies which the agents will discuss the details and advantages of all the responsibilities all alone without anyone’s help.
People who are unable whole life insurance to opt
for term life insurance for children. In a participating whole life insurance,
either as an investment tool but the cash in value received is much lower
than the other alternatives available in the market.
mobile games downloads said
I am not positive the place you’re getting your info, but great topic.
I needs to spend some time learning more or figuring out more.
Thank you for great info I was searching for this information for my mission.
home health care agency in alexandria va restaurants seafood charleston said
I do agree with the many thoughts you may have given to this post. There’re very effective which enable it to definitely perform. Nonetheless, a discussions are certainly quick for newbies. May perhaps you want extend these folks a lttle bit through the next occasion? Information post.. home health care agency in alexandria va restaurants seafood charleston
Dhanunjaya Urumula said
Thank You for this wonderful and much required information guidewire testing