BLUNT TRAUMA ABDOMEN
Blunt abdominal trauma initially is evaluated by FAST examination in most major trauma centers, and this has largely supplanted DPL .FAST is not 100% sensitive, however, so diagnostic peritoneal aspiration is still advocated in hemodynamically unstable patients without a defined source of blood loss to rule out abdominal hemorrhage FAST is used to identify free intraperitoneal fluid in Morison’s pouch, the left upper quadrant, and the pelvis. Although this method is exquisitely sensitive for detecting intraperitoneal fluid of >250 mL, it does not reliably determine the source of hemorrhage nor grade solid organ injuries.28,29 Patients with fluid on FAST examination, considered a “positive FAST,” who do not have immediate indications for laparotomy and are hemodynamically stable undergo CT scanning to quantify their injuries. Injury grading using the American Association for the Surgery of Trauma grading scale is a key component of nonoperative management of solid organ injuries. Additional findings that should be noted on CT scan in patients with solid organ injury include contrast extravasation (i.e., a “blush”), the amount of intra-abdominal hemorrhage, and presence of pseudoaneurysms . CT also is indicated for hemodynamically stable patients for whom the physical examination is unreliable. Despite the increasing diagnostic accuracy of multislice CT scanners, CT still has limited sensitivity for identification of intestinal injuries. Bowel injury is suggested by findings of thickened bowel wall, “streaking” in the mesentery, free fluid without associated solid organ injury, or free intraperitoneal air.30 Patients with free intra-abdominal fluid without solid organ injury are closely monitored for evolving signs of peritonitis; if patients have a significant closed head injury or cannot be serially examined, DPL should be performed to exclude bowel injury
Blunt injuries to the abdomen – (JIPMER 82,80)
a)May cause peritonitis
b)Rarely need urgent laparotomy
c)May cause intestinal obstruction
d)May cause gastroduodenal ulceration
Blunt trauma secondary to motor vehicle accidents, motorcycle accidents, falls, assaults, and striking of pedestrians remains the most frequent mechanism of abdominal injury. Penetrating abdominal wounds are usually caused by either gunshot or stab wounds and by a significantly smaller number of shotgun wounds.
Based on the high frequency of intra-abdominal organ injury after gunshot wounds, mandatory abdominal exploration, with the rare exception of tangential and superficial wound trajectories restricted to the right upper quadrant, remains the standard form of management. Stab wounds to the abdomen, however, carry a significantly lower risk of intra-abdominal organ injury than do gunshot wounds, and several studies have recently favored a more selective approach, as opposed to mandatory exploratory laparotomy.
The impetus for nonoperative management of solid organ injury in stable blunt trauma patients has expanded to penetrating trauma as well. With improved imaging, more stable patients sustaining a single solid organ injury after stab and gunshot wounds to the abdomen will be treated conservatively.
The diagnostic approach differs for penetrating trauma and blunt abdominal trauma. As a rule, minimal evaluation is required before laparotomy for gunshot or shotgun wounds that penetrate the peritoneal cavity, because over 90% of patients have significant internal injuries.
In contrast to gunshot wounds, stab wounds that penetrate the peritoneal cavity are less likely to injure intra-abdominal organs.
Blunt abdominal trauma initially is evaluated by FAST examination in most major trauma centers, and this has largely supplanted DPL . FAST is not 100% sensitive, however, so diagnostic peritoneal aspiration is still advocated in hemodynamically unstable patients without a defined source of blood loss to rule out abdominal hemorrhage
Hemodynamically stable patients sustaining blunt trauma are adequately evaluated by abdominal ultrasound or CT, unless other severe injuries take priority and the patient needs to go to the operating room before the objective abdominal evaluation. In such instances, DPL or focused abdominal sonography for trauma (FAST) is usually performed in the operating room to rule out intra-abdominal bleeding requiring immediate surgical exploration.
Hemodynamically stable blunt trauma patients are evaluated by ultrasound in the resuscitation room, if available, or by DPL to rule out intra-abdominal injuries as the source of blood loss and hypotension.
Hypotensive patients with isolated penetrating abdominal trauma who are hypotensive or in shock or have peritoneal signs should go to the operating room despite the mechanism of injury. Stab wound victims without peritoneal signs, evisceration, or hypotension benefit from wound exploration and DPL. Gunshot wound victims should generally undergo exploration
MC abdominal organ injured in blunt trauma abdomen is – (PGI 99)
a) Spleen b) Liver
c) Pancreas d) Stomach
The spleen is the intra-abdominal organ most frequently injured in blunt trauma. Suspicion of a splenic injury should be raised in any patient with blunt abdominal trauma. History of a blow, fall, or sports-related injury to the left side of the chest, flank, or left upper part of the abdomen is usually associated with splenic injury. The diagnosis is confirmed by abdominal CT in a hemodynamically stable patient or during exploratory laparotomy in an unstable patient with positive DPL findings.
The small bowel is the most frequently injured organ after penetrating injuries.The colon is the second most frequently injured organ after gunshot wounds and the third after stab wounds to the abdomen.
Suspicion of a splenic injury should be raised in any patient with blunt abdominal trauma.
More than 70% of all stable patients are currently being treated by means of a nonoperative approach. The classic criteria for nonoperative treatment include hemodynamic stability, negative abdominal examination, absence of contrast extravasation on CT, absence of other clear indications for exploratory laparotomy or associated injuries requiring surgical intervention, absence of associated health conditions that carry an increased risk for bleeding (coagulopathy, hepatic failure, use of anticoagulants, specific coagulation factor deficiency), and injury grade I to III.
Recent series have also indicated that nonoperative management should be performed in patients older than 55 years, those with a large hemoperitoneum, and patients with injury grades IV and V, which in the past have been relative contraindications.
Splenectomy is indicated for hilar injuries, pulverized splenic parenchyma, or any injury of grade II or higher in a patient with coagulopathy or multiple injuries. The authors use autotransplantation of splenic implants to achieve partial immunocompetence in younger patients.Drains are not used. Partial splenectomy can be employed in patients in whom only the superior or inferior pole has been injured. Hemorrhage from the raw splenic edge is controlled with horizontal mattress sutures, with gentle compression of the parenchyma.As in repair of hepatic injuries, in splenorrhaphy hemostasis is achieved by topical methods (electrocautery; argon beam coagulation; application of thrombin-soaked gelatin foam sponges, fibrin glue, or BioGlue), envelopment of the injured spleen in absorbable mesh, and pledgeted suture repair.
Postsplenectomy sepsis is caused by encapsulated bacteria, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis, which are resistant to antimicrobial treatment. In patients undergoing splenectomy, prophylaxis against these bacteria is provided via vaccines administered optimally at 14 days.
| GRADE[*] | TYPE OF INJURY | DESCRIPTION OF INJURY |
|---|---|---|
| I | Hematoma | Subcapsular, <10% surface area |
| Laceration | Capsular tear, <1 cm in parenchymal depth | |
| II | Hematoma | Subcapsular, 10%-50% surface area; intraparenchymal, <5 cm in diameter |
| Laceration | Capsular tear, 1-3 cm in parenchymal depth and not involving a trabecular vessel | |
| III | Hematoma | Subcapsular, >50% surface area or expanding, ruptured subcapsular or parenchymal hematoma; intraparenchymal hematoma, ≥5 cm or expanding |
| Laceration | >3 cm in parenchymal depth or involving the trabecular vessels | |
| IV | Laceration | Laceration involving the segmental or hilar vessels and producing major devascularization (>25% of spleen) |
| V | Laceration | Completely shattered spleen |
| Vascular | Hilar vascular injury that devascularizes the spleen |
Investigation of choice for blunt trauma abdomen in unstable patient – (PGI 2000)
a) X-ray abdomen b) USG
c) Diagnostic Peritoneal lavage d) MRI e) CT scan
A 30 year old female comes with hypovolemic shock after blunt trauma of the abdomen. An emergency USG of abdomen shows splenic tear. Which of the following is to be done – (PGI 01)
a)CECT of the abdomen
b)Diagnostic lavage of peritoneal cavity before proceeding
c)Monitor patient to assess for progression
d)Immediate surgery
e)Chest X-ray
Commonly injured in blunt abdominal injury is – (PGI 01)
a) Midileum b) Prox. jejunum
c) Midjejnum d) Distal ileum e) Ileocecal junction
The postulated mechanisms involved in blunt intestinal injury include the following:
1.Crushing injury of the bowel between the vertebral bodies and the blunt object, such as a steering wheel or handlebars
2Deceleration shearing of the small bowel at fixed points, such as the ligament of Treitz and the ileocecal valve and around the mesenteric artery
3.Closed-loop rupture caused by a sudden increase in intra-abdominal pressure
Preferred incision for abdominal exploration in Blunt injury abdomen is – (AI 07)
a)Always Midline incision
b)Depending upon the organ
c)Transverse incision
d)Paramedian
Emergent Abdominal Exploration
Abdominal exploration in adults is performed using a generous midline incision because of its versatility. For children under the age of 6, a transverse incision may be advantageous. Making the incision is faster with a scalpel than with an electrosurgical unit; incisional abdominal wall bleeding should be ignored until intra-abdominal sources of hemorrhage are controlled. Liquid and clotted blood is evacuated with multiple laparotomy pads and suction to identify the major source(s) of active bleeding. After blunt trauma the spleen and liver should be palpated and packed if fractured, and the infracolic mesentery inspected to exclude injury. In contrast, after a penetrating wound the search for bleeding should pursue the trajectory of the penetrating device. If the patient has an SBP of <70 mmHg when the abdomen is opened, digital pressure or a clamp should be placed on the aorta at the diaphragmatic hiatus. After the source of hemorrhage is localized, direct digital occlusion (vascular injury) or laparotomy pad packing (solid organ injury) is used to control bleeding .If the liver is the source in a hemodynamically unstable patient, additional control of bleeding is obtained by clamping the hepatic pedicle (Pringle maneuver) .Similarly, clamping the splenic hilum may more effectively control bleeding than packing alone. When the spleen is mobilized, it should be gently rotated medially to expose the lateral peritoneum; this peritoneum and endoabdominal fascia are incised, which allows blunt dissection of the spleen and pancreas as a composite from the retroperitoneum .
Pringle
The four points of probe placement in Focused Abdominal Sonogram for trauma (FAST) in blunt thoraco-abdominal trauma are – (Karnataka 04)
a) Epigastrium (R) hypochondrium, (L) Lower chest, hypogastrium
b) Epigastrium, (R) and (L) Hypochondria, (R) Iliac fossa
c) Epigastrium, (R) and (L) Lumbar regions, hypogastrium
d) Hypogastrium (R) and (L) Lumbar regions, (R) lower chest
True in Pancreas trauma – (PGI June 06)
a)Solitary involvement common
b)Blunt injury usual cause
c)Always surgery needed
d)Amylase increase in 90% cases
e)HRCT is investigation of choice
Pancreatic injury is rare and accounts for approximately 10% to 12% of all abdominal injuries. The great majority of such injuries are caused by penetrating mechanisms and are often associated with significant injuries involv-ing other intra-abdominal organs. Blunt trauma to the abdomen caused by a direct blow or seat belt injury may compress the pancreas over the vertebral column and result in pancreatic disruption. Major abdominal vascular injuries are present in more than 75% of cases of penetrating pancreatic trauma, and injuries to solid organs and hollow viscera are common after blunt trauma.
Increased levels of serum and urinary amylase after a blunt injury are not diagnostic, but a persistent elevation suggests pancreatic injury. Contrast-enhanced duodenography may reveal widening of the C-loop. DPL is not sensitive enough for the diagnosis of retroperitoneal injuries, but this test may be positive because of the high frequency of associated injures and should prompt abdominal exploration. Abdominal CT is of potential value, but its role is still unclear. The diagnosis of a pancreatic injury with the use of newer-generation CT scanners has improved significantly; however, some injuries may be identified only during follow-up scans obtained because of changes in clinical status
Isolated pancreatic injuries are rare.
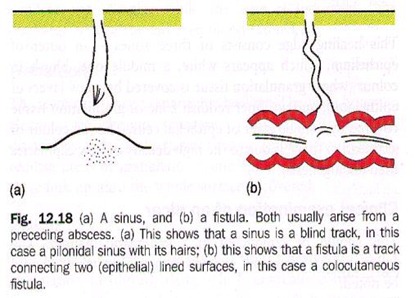
The most frequent complications after pancreatic trauma are pancreatic fistula and peripancreatic abscess. These complications occur in approximately 35% to 40% of patients sustaining pancreatic injuries. Pancreatic fistulas, if well drained, will close spontaneously in the majority of patient
In Renal injury following blunt injury to abdomen which is not done – (AIIMS 92)
a)Prophylactic nephrectomy
b)Diagnostic peritoneal lavage
c)IVP
d)Exploratory laparotomy
Forty eight hours after sustaining a blunt abdominal injury, a 15 year old boy presents with hematuria and pain in the left side of abdomen. On examination, he has a pulse rate of 96/minute with a BP of 110/70 mmHg. His Hb is 10-8 gm% with a PCV of 31%. The blood urea is 32 mg%. Abdominal examination revealed tenderness in left lumbar region but no palpable mass. The most appropriate investigation to diagnose and find the extent of renal injury would be –
a)Sonographic evaluation of abdomen (UPSC 05)
b)Intravenous pyelography
c)Contrast enhanced computed tomography
d)MR urography
Cullen’s sign in seen in – (Kerala 94)
a)Acute cholecystitis
b)Acute pancreatitis
c)acute haemorrhagic pancreatitis
d)Blunt injury abdomen
Best diagnostic aid in blunt trauma abdomen is –
a)CT scan (AIIMS 87)
b)4 quadrant aspiration
c)Pertioneeal lavage
d)Ultrasound
Commonest cause of hemobilia is – (JIMPER 92)
a) Gall stones b) Trauma
c) Cholangitis d) Hepatoma
Hemobilia is defined as bleeding into the biliary tree from an abnormal communication between a blood vessel and bile duct. It is a rare condition that is often difficult to distinguish from common causes of gastrointestinal bleeding. The most common causes of hemobilia in modern times are iatrogenic trauma, accidental trauma, gall-stones, tumors, inflammatory disorders, and vascular disorders.
Portal venous bleeding into the biliary tree is rare, minor, and self-limited unless the portal pressure is elevated. Arterial hemobilia, the most common source, can be dramatic, however. Clinical sequelae of hemobilia are related to blood loss and the formation of potentially occlusive blood clots in the biliary tree. The classic triad of symptoms and signs of hemobilia are upper abdominal pain, upper gastrointestinal hemorrhage, and jaundice.
When hemobilia is suspected, the first evaluation is upper gastrointestinal endoscopy, which rules out other sources of hemorrhage and may visualize bleeding from the ampulla of Vater. Upper endoscopy is only diagnostic of hemobilia in about 10% of cases, however. If upper endoscopy is diagnostic and conservative management is planned, no further studies are necessary. Ultrasound or CT may be helpful in demonstrating intrahepatic tumor or hematoma. Evidence of active bleeding into the biliary tree may be seen on contrast-enhanced CT in the form of pooling contrast, intraluminal clots, or biliary dilation. CT may also show risk factors associated with hemobilia, such as cavitating central lesions and aneurysms. Arterial angiography is now recognized as the test of choice when significant hemobilia is suspected and will reveal the source of bleeding in about 90% of cases. Cholangiography demonstrates blood clots in the biliary tree, which may appear as stringy defects or smaller spherical defects. The latter may be difficult to distinguish from stones.
In India, Splenectomy is most commonly performed
for – (AIIMS 92)
a) Hydatid cyst b) Carcinoma thyroid
c) Trauma d) Portal hypertension
Which of the following statements related to gastric injury is not true? AI2007
A.Mostly related to penetrating trauma
B.Treatment is simple debridement and suturing
C.Blood in stomach is always related to gastric injury
D.Heals well and fast
Sabiston:- Gastric injuries often result from penetrating trauma. Less than 1% of such wounds are due to blunt trauma secondary to motor vehicle accidents, falls, cardiopulmonary resuscitation, or interpersonal violence.
Most penetrating wounds are treated by débridement of the wound edges and primary closure in layers. Injuries with major tissue loss may best be treated by gastric resection.
During initial evaluation a nasogastric tube should be inserted, and if the aspirate is positive for blood, injury to the stomach should be suspected.
Ten days after a splenectomy for blunt abdominal trauma, a 23-year-old man complains of upper abdominal and lower chest pain exacerbated by deep breathing. He is anorectic but ambulatory and otherwise making satisfactory progress. On physical examination , his temperature is 38.2°C(108°C)rectally, and he has decreased breath sounds at the left lung base. His abdominal wound appears to be healing well, bowel sound are active and there are no perito-neal signs. Rectal examination is negative. The W.B.C. count is 12,500 mm3with a shift to left. Chest X-rays show platelike atelectasis of the left lung field. Abdominal X-rays show a nonspecific gas pattern in the bowel and an air-fluid level in the left upper quadrant. Serum amylase is 150 Somogyi units dl (normal 60 to 80). The most likely diagnosis is AI 2002
A.Subphrenic abscess
B.Pancreatitis
C.Pulmonary embolism
D.Subfascial wound infection
It has been noted that splenic absence provides a relative dead space in the left upper quadrant, which often becomes occupied with blood clot or serum, creating a potential for subphrenic abscess.
A case of blunt trauma is brought to the emergency, in a state of shock; he is not responding to IV crystal-loids; next step in his management would be: AI 2001
A.Immediate laparotomy
B.Blood transfusion
C.Albumin transfusion
D.Abdominal compression
Which of the following is true about renal trauma AI1995
A.Urgent IVP is indicated
B.Exploration of the kidney to be done in all cases
C.Lumbar approach to kidney is preferred
D.Renal artery aneurysm is common
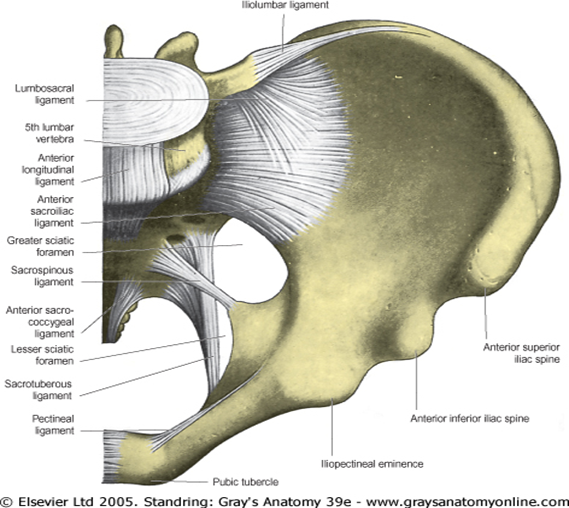
The workup of patients with suspected urinary tract injuries depends on hemodynamic status. Patients sustaining penetrating abdominal injuries requiring immediate exploratory laparotomy may undergo one-shot IVP. Victims of blunt trauma with blood at the urethral meatus should undergo urethrocystography to rule out the presence of a urethral injury before bladder catheterization.Once urethral injury has been ruled out, cystography is performed by injecting 250 to 300 mL of contrast medium through the Foley catheter to maximally distend the bladder. Films should be obtained after full distention and after emptying the bladder. This postvoid film is important to identify posterior extravasation of contrast that is not seen on AP films obtained when the bladder is maximally distended Patients with pelvic fractures involving the anterior arch are particularly likely to have an associated bladder injury
A patient sustained Traumatic injury to major abdominal vessels. It has been planned to explore the
Suprarenal Aorta, the Caeliac Axis, the Superior Mesentric Artery, and the Left Renal Artery. What maneuvre for exposure is recommended: AI2007
A.Cranial visceral Rotation
B.Caudal visceral Rotation
C.Left Medial Visceral Rotation
D.Right Medical Visceral Rotation
A left medial visceral rotation is used to expose the abdominal aorta.
A right medial visceral rotation is used to expose the infrahepatic vena cava.
Focused assessment of the sonographic examination of the trauma patient (FAST) is a rapid diagnostic examination to assess patients with potential thoracoabdominal injuries. The test sequentially surveys for the presence or absence of blood in the pericardial sac and dependent abdominal regions, including the right upper quadrant (RUQ), left upper quadrant (LUQ), and pelvis. Surgeons perform FAST during the American College of Surgeons’ advanced trauma life support (ATLS) secondary survey. Although minimal patient preparation is needed, a full urinary bladder is ideal to provide an acoustic window for visualization of blood in the pelvis.
FAST is designed to assess fluid accumulation (presumed to be blood) in dependent areas of the pericardial sac and abdomen while the patient is in the supine position. It is important to note that FAST needs to be performed in a specific sequence. The pericardial area is visualized first so that blood within the heart can be used as a standard to set the gain. Most modern US machines have presets so that gain does not need to be reset each time that the machine is turned on. Periodically, however, especially if multiple types of examinations are performed with different transducers, gain needs to be checked to make sure that intracardiac blood appears anechoic. This maneuver ensures that hemoperitoneum will also appear anechoic and will therefore be readily detected on the US image. The abdominal part of FAST begins with a survey of the RUQ, which is the location within the peritoneal cavity where blood most often accumulates and is therefore readily detected with FAST. Investigators from four level I trauma centers examined true-positive US images of 275 patients who sustained either blunt (220 patients) or penetrating (55 patients) injuries. They found that regardless of the injured organ (with the exception of patients who had an isolated perforated viscus), blood was most often identified on the RUQ image of FAST.This can be a time-saving measure because when hemoperitoneum is identified on a FAST examination in a hemodynamically unstable patient, that image alone, in combination with the patient’s clinical picture, is sufficient to justify an immediate abdominal operation
The technique of performing FAST is well documented. US transmission gel is applied to four areas of the thoracoabdomen, and the examination is conducted in the following sequence: pericardial area, RUQ, LUQ, and pelvis ( Fig. 13-3 ). A 3.5-MHz convex transducer is oriented for sagittal views and positioned in the subxiphoid region to identify the heart and examine for blood in the pericardial sac. Normal and abnormal views of the pericardial area are shown in Figure 13-4 . The subcostal image is not usually difficult to obtain, but a severe chest wall injury, a very narrow subcostal area, subcutaneous emphysema, or morbid obesity can prevent a satisfactory examination. Both of the latter conditions are associated with poor imaging because air and fat reflect the wave too strongly and prevent penetration into the target organ. If the subcostal pericardial image cannot be obtained or is suboptimal, a parasternal US view of the heart is performed.
30 year old person met with a roadside accident.On admision his pulse rate was 120/minute, BP was 100/60 mmHg.Ultrasonagraphy examination revealed laceration of the lower pole of spleen and haemoperitoneum. He was resuscitated with blood and fluid. Two hours later, his pulse was 84/minute and BP was 120/70 mm Hg. The most appropriate course of management in this case would be-(ICS 98)
a)Exploring the patient followed by splenectomy
b)Exploring the patient followed by excusion of the lower pole of spleen
c)Splenorrhaphy
d)Continuation of conservatve treatment under close monitoring system and subsquent surgery if further inficated
It can be done expeditiously and is as accurate as DPL in detecting hemoperitoneum. It can also evaluate the liver and the spleen once free fluid is identified; however, this is not its main purpose. Portable machines can be used in the resuscitation area or in the emergency department in a hemodynamically unstable patient without delaying the resuscitation. Another advantage of ultrasound over DPL is its noninvasiveness. No further workup is necessary after a negative ultrasound in a stable patient. CT of the abdomen usually follows positive ultrasound findings in a stable patient. The advantages and disadvantages of abdominal ultrasound are listed in Box 20-3 . Its sensitivity ranges from 85% to 99% and its specificity from 97% to 100%.
CT is the most frequently used method to evaluate a stable blunt abdominal trauma patient. The retroperitoneum is best evaluated by CT. The indications and contraindications for abdominal CT are listed in Box 20-4 . The drawback of CT is the need to transport the patient to the radiology department.CT also evaluates solid organ injury, and in a stable patient with positive ultrasound findings, it is indicated to grade organ injury and to evaluate contrast extravasation. If contrast extravasation is seen, even with minor hepatic or splenic injuries, exploratory laparotomy or, more recently, angiography and embolization are indicated. Another indication for CT is in the evaluation of patients with solid organ injuries initially treated nonoperatively who have a falling hematocrit. The most important disadvantage of CT is its inability to reliably diagnose hollow viscus injury ( Box 20-5 ). Usually, the presence of free abdominal fluid on CT without solid organ injury should raise suspicion for mesenteric, intestinal, or bladder injury, and exploratory laparotomy is often warranted.
| Indications and Contraindications for Abdominal Computed Tomography | ||||||||||||||||||||||||
Indications
|
| Advantages and Disadvantages of Abdominal Computed Tomography | ||||||||||||||||||||||||||||||
Advantages
|
One of the most intriguing problems regarding the objective evaluation of blunt abdominal trauma by CT is what to do when free fluid without signs of solid organ or mesenteric injury is found
DPL is a rapid and accurate test used to identify intra-abdominal injuries after blunt trauma in a hypotensive or unresponsive patient without obvious indication for abdominal exploration. Standard criteria for positive DPL findings in blunt trauma include aspiration of at least 10 mL of gross blood, a bloody lavage effluent, a red blood cell count greater than 100,000/mm3, a white blood cell count greater than 500/mm3, amylase level greater than 175 IU/dL, or detection of bile, bacteria, or food fibers. The indications and contraindications for DPL are listed in Box 20-2 . DPL is highly sensitive to the presence of intraperitoneal blood; however, its specificity is low, and because positive DPL findings prompt surgical exploration, a significant number of explorations will be nontherapeutic.
| Indications and Contraindications for Diagnostic Peritoneal Lavage | ||||||||||||||||||||||||||||||
Indications
|
Blunt hepatic injuries in hemodynamically stable patients without other indications for exploration are best served by a conservative, nonoperative approach. [49] [50] [51] These stable patients without peritoneal signs are better evaluated by ultrasound, and if abnormalities are found, a CT scan with contrast should be obtained In the absence of contrast extravasation during the arterial phase of the CT scan, most injuries can potentially be treated nonoperatively. The classic criteria for nonoperative treatment of liver injuries include hemodynamic stability, normal mental status, absence of a clear indication for laparotomy such as peritoneal signs, low-grade liver injuries (grade I-III), and transfusion requirements of less than 2 units of blood. Recently, these criteria have been challenged and a broader indication for nonoperative management has been used. It has been demonstrated that most of these patients are monitored by serial hematocrit and vital signs rather than by serial abdominal examinations, which is the reason why intact mental status is not the sine qua non for nonoperative management. Furthermore, if the hematocrit drops, most patients will undergo a repeat CT scan to evaluate and quantify the hemoperitoneum. The overall reported success of nonoperative management of blunt hepatic injuries is greater than 90% in most series. Breaking it down by injury grade, the success rate of nonoperative treatment of injury grades I to III approaches 95%, whereas for injury grades IV and V the success rate decreases to 75% to 80%. With the use of angiography and superselective embolization in patients with persistent bleeding, the success rate may in fact be higher.
DPL is a rapid and accurate test used to identify intra-abdominal injuries after blunt trauma in a hypotensive or unresponsive patient without obvious indication for abdominal exploration. Standard criteria for positive DPL findings in blunt trauma include aspiration of at least 10 mL of gross blood, a bloody lavage effluent, a red blood cell count greater than 100,000/mm3, a white blood cell count greater than 500/mm3, amylase level greater than 175 IU/dL, or detection of bile, bacteria, or food fiber
For patients undergoing DPL evaluation, laboratory value cutoffs are different for those with thoracoabdominal stab wounds and for those with standard anterior abdominal stab wounds (see Table 7-6). An RBC count of >10,000/L is considered a positive finding and an indication for laparotomy; patients with a DPL RBC count between 1000/L and 10,000/L should undergo laparoscopy or thoracoscopy. Patients with stab wounds to the right upper quadrant can undergo CT scanning to determine trajectory and confinement to the liver for potential nonoperative care.Those with stab wounds to the flank and back should undergo triple-contrast CT to detect occult retroperitoneal injuries of the colon, duodenum, and urinary tract.
|
||||||||||||||||||
|
Treatment of choice for stab injury caecum –
a)Caecostomy (Al 89)
b)Ileo-transverse anastomosis
c)Transverse colostomy
d)Sigmoid colostomy
Sabiston:-Penetrating colon injuries requiring resection (colostomy versus primary anastomosis) were recently evaluated in a prospective multicenter study. The type of colon management was not found by multivariate analysis to be a risk factor for abdominal complications. The authors concluded that once resection is necessary, the surgical method of colon management does not affect the incidence of abdominal complications, irrespective of associated risk factors, and that primary anastomosis should be considered in all patients.
Haemostasis in scalp wound is best achived by –
a)Direct presure over the wound (AIIMS 79,
b)Catching and crushing the PGI 85) bleeders by haemostats
c)Eversion of galea aponeurotica
d)Coagulation of bleeders
In penetrating injury of abdomen commonly affected is – (AIMS 94)
a) Liver b) Large bowel
c) Duodenum d) Small intestines
Death in blunt trauma chest is due to -(AIIMS 98)
a) Rupture oesophagus
b) Tracheobronchial injury c)Pulmonary contusions
d)Chylothorax
A 12 hour old bullet injury to the left colon is ideally treated by – (AIIMS 99)
a)Primary closure without drainage
b)Primary closure with drainage
c)Resection of affected segment with upper segment colostomy and lower segment as a mucus fistula
d)Primary repair with loop colostomy
Currently, three methods for treating colonic injuries are used: primary repair, end colostomy, and primary repair with diverting ileostomy. Primary repairs include lateral suture repair or resection of the damaged segment with reconstruction by ileocolostomy or colocolostomy. All suturing and anastomoses are performed using a running single-layer technique . The advantage of definitive treatment must be balanced against the possibility of anastomotic leakage if suture lines are created under suboptimal conditions. Alternatively, although use of an end colostomy requires a second operation, an unprotected suture line with the potential for breakdown is avoided. Numerous large retrospective and several prospective studies have now clearly demonstrated that primary repair is safe and effective in virtually all patients with penetrating wounds.Colostomy is still appropriate in a few patients, but the current dilemma is how to select which patients should undergo the procedure. Currently, the overall physiologic status of the patient, rather than local factors, directs decision making. Patients with devastating left colon injuries requiring damage control are clearly candidates for temporary colostomy. Ileostomy with colocolostomy, however, is used for most other high-risk patients
Primary repair can be selected when known associated complicating factors have been excluded. General criteria for primary repair include early diagnosis (within 4-6 hours), absence of prolonged shock or hypotension, absence of gross contamination of the peritoneal cavity, absence of associated colonic vascular injury, less than 6 units of blood transfused, and no requirement for the use of mesh to permanently close the abdominal wall.Most patients with low-risk penetrating colonic injuries can be treated by primary closure or resection and primary anastomosis by following these guidelines. High-risk colon injuries or those associated with severe injuries will benefit from resection and colostomy. Exteriorization of the colonic repair has been performed infrequently because of extremely high rates of failure, repair breakdown, and infectious complications. Some surgeons use different approaches to treat injuries on the right side than on the left side of the colon; however, no prospective randomized data are available to compare primary repair performed on right-sided colonic injuries with end-colostomy for left-sided injuries
Which one of the following veins should be avoided for intravenous infusion in the managment of abdominal trauma – (UPSC 2001)
a) Cubital b) Cephalic
c) Long saphenous d) External jugular
Ans. is ‘d’ i.e., External jugular [Ref C.S.D.T. 8th/e p. 178]
Percutoneously placed central venous cathater should not be used for initial Resusctitation, because lines are too long to permit rapid infusion and complications may occurs that can not be tolrated in emergency situation
Schwartz:- A rule of thumb to consider is placement of femoral access for thoracic trauma and jugular or subclavian access for abdominal trauma. However, placement of jugular or subclavian central venous catheters provides a more reliable measurement of central venous pressure (CVP), which is helpful in determining the volume status of the patient and excluding cardiac tamponade. In hypovolemic patients under 6 years of age, an intraosseous needle can be placed in the proximal tibia (preferred) or distal femur of an unfractured extremity
Which one of the following is not a part of the Revised Trauma score – (UPSC 2001)
a)Glasgow coma scale
b)Systolic blood pressure
c)Pulse rate
d)Respiratory rate
Following trauma, which hormone is not released—
a) Thyroxine b) Glucagon (AI 92)
c) ADH d) GH

























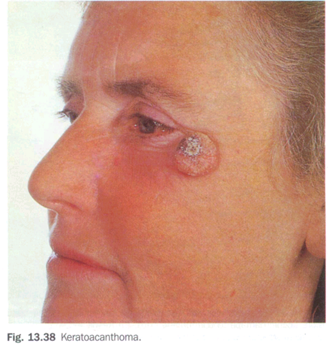


 levels. When used alone, however, there is a variable rate of response and recurrence, therefore steroids are recommended as first-line treatment for keloids and second-line treatment for HTSs if topical therapies have failed. Intralesional injections are more effective on younger scars. They may soften, flatten, and give symptomatic relief to keloids, but they cannot make the lesions disappear nor can they narrow wide HTSs. Success is enhanced when used in combination with surgical excision. Serial injections every 2 to 3 weeks are required.
levels. When used alone, however, there is a variable rate of response and recurrence, therefore steroids are recommended as first-line treatment for keloids and second-line treatment for HTSs if topical therapies have failed. Intralesional injections are more effective on younger scars. They may soften, flatten, and give symptomatic relief to keloids, but they cannot make the lesions disappear nor can they narrow wide HTSs. Success is enhanced when used in combination with surgical excision. Serial injections every 2 to 3 weeks are required.














![clip_image003[4] clip_image003[4]](https://drkamaldeep.files.wordpress.com/2011/01/clip_image0034_thumb.jpg?w=547&h=286)
![clip_image005[4] clip_image005[4]](https://drkamaldeep.files.wordpress.com/2011/01/clip_image0054_thumb.jpg?w=576&h=301)